
MedFriendly®


Colposcopy
A colposcopy is a visual examination of the vagina
and cervix with a lighted magnifying instrument,
known as a colposcope. The vagina is an opening in
the female's body that is part of the reproductive
system. The cervix is a small, cylinder-shaped organ
that forms the lower part and neck of the uterus. The
uterus is a hollow organ in a female's body where the
egg is implanted and the baby to be develops. A
colposcopy is considered by doctors to be a simple
procedure.
FEATURED BOOK: Colposcopy, Principles, and
The aspects of a colposcopy.
WHEN AND WHY IS A COLPOSCOPY PERFORMED?
A colposcopy is mainly performed after results of a Papanicolaou's (Pap) smear have
come back abnormal. A Pap smear is a type of test used to detect abnormal changes in
cells. This is done by scraping away loose cells from the cervix, spreading (smearing) it
on a glass slide, and examining it under a microscope.
A Pap smear (and a colposcopy) is used to detect and prevent the development of
cervical cancer (cancer of the cervix) by identifying cells that may become cancerous in
the future. Cancer is an abnormal growth of new tissue characterized by uncontrolled
growth of abnormally structured cells that have a more primitive form. Detection of
abnormal cells in the cervix can help prevent and treat cancer of the cervix.
"Where Medical Information is Easy to Understand"™
Most abnormal Pap smear results usually do not represent cancer.
Rather, most abnormal Pap smear results represent inflammation
or infection. A Pap smear is not used to diagnose cancer. Rather,
a Pap smear is used as a screening test, meaning that it identifies
(screens) abnormal changes in cells that may be cancerous now
or in the future.
Pap smears can identify abnormal changes in cells long before
invasive cancer develops. After a Pap smear is performed,
appropriate follow-up care needs to be undertaken to determine
what the abnormal results mean. This is where a colposcopy
comes in.
A colposcopy is used after a Pap smear because it provides a more detailed look at the suspected
abnormal area or areas. Thus, a colposcopy is used as a type of follow-up examination that is more
sensitive than the Pap smear. Unlike a Pap smear, a colposcopy is not a screening test. A colposcopy is
called a diagnostic test because it helps to identify the cause of the abnormal Pap smear results, which
leads to a diagnosis of the disease or condition that is present. The severity of the abnormality can also
be determined during a colposcopy.
The type of cells that come back as abnormal on a Pap smear result are often flat cells known as
squamous cells. The doctor is often not sure if the abnormal results are serious or not. The term used to
describe this type of abnormal result is ASCUS (abnormal squamous cells of uncertain significance).
A colposcopy is often used to follow up on other abnormal Pap smear findings such low-grade or high-
grade squamous intraepithelial lesions, koliocytosis, higher grade squamous cell carcinomas, or
carcinoma in situ. A squamous intraepithelial lesion refers to abnormalities in squamous intraepithelium
that may be moderate or severe, but it does not mean that cancer is present. Squamous intraepithelium
is a sheet of scaly cells that are attached together at the edges. A low grade abnormality means that it is
usually less serious than a high grade abnormality.
Koilocytosis refers to the presence of squamous cells that often have two nuclei and small holes near
the nuclei. Nuclei means more than one nucleus. The nucleus is the center of a cell. The presence of
koiliocytosis is characteristic of the human papillomavirus (HPV) infection. HPV is a type of virus that
causes warts on the hands and feet and damage to the mucous membranes of the mouth, anus, and
genital (private part) openings. A wart is a growth on the body caused by a virus. A mucous membrane is
one of four major types of thin sheets of tissue that line or cover various parts of the body.
A carcinoma is any malignant cancer that arises from cells in the covering surface layer or membrane
(outer covering) that lines an organ of the body. When describing cancer, malignant means that the
newly formed tissues are made of abnormally structured and primitive-looking cells that grow
uncontrollably, spread throughout the body, and invade surrounding tissues. A squamous cell carcinoma
refers to carcinoma of the squamous cells. Carcinoma in situ refers to abnormal cells that are not yet
malignant but show signs of cancer.
The doctor may also want to perform a colposcopy if the patient was exposed to diethylstilbestrol (DES)
as baby. DES is an artificially manufactured hormone. Hormones are natural chemicals produced by the
body and released into the blood that have a specific effect on tissues in the body. Artificial hormones
are not naturally produced by the body but have similar effects as natural hormones. Many mothers took
DES between 1938 and 1971, believing they were taking vitamins. DES is not a vitamin, however, and
causes severe health risks and consequences in the mothers that used it and in their children.
Even without abnormal Pap smear results, a gynecologist may look at the cervix, vagina, or outer genital
area with the naked eye and notice an abnormal appearance, prompting him/her to do a colposcopy to
get a closer look. A gynecologist is a physician (medical doctor) who specializes in the health care of
women, including diseases and normal physical care of the female reproductive system.
WHEN IS A BIOPSY PERFORMED?
If any abnormal areas are seen during the colposcopy, a biopsy is performed. A biopsy is the process of
removing living tissue or cells from organs or other body parts of patients for examination under a
microscope or in a culture to help make a diagnosis, follow the course of a disease, or estimate a
prognosis. A culture is an artificial way to grow cells or tissues in the laboratory.
A colposcopy helps magnify abnormal areas of the cervix when a biopsy needs to be performed so that it
can be done precisely. A special device that looks like a bird's beak is used to remove tissue samples
from the worst looking area. Only abnormal tissue samples need to be taken with a biopsy of the cervix.
The tissue sample is usually an eighth of an inch deep. If there are multiple areas that need to be
biopsied, tissue samples are taken from the area farthest back in the cervix. This prevents bleeding over
other areas in the front that may need to be biopsied. Biopsy results usually take two to three days but
can take as long as one to two weeks.
Before or after a biopsy is performed, many doctors perform a procedure known as endocervical
curettage (ECC). ECC is the removal of tissue from the inside of the cervix with a spoon-shaped
instrument known as a curetta. An ECC can help the doctor determine if there are abnormalities inside
the canal (passageway) of the cervix that cannot be seen.
If any abnormal areas are in the canal of the cervix, or if the entire abnormal area cannot be viewed, a
cone biopsy is often performed. A cone biopsy is removal of a cone shaped section of the cervix to be
analyzed under a microscope. The doctor will take notes to record the locations where biopsies were
taken from. Each tissue sample is placed in a jar and labeled according to the location where it was
taken from.
WILL THE DOCTOR DESTROY ABNORMAL TISSUES DURING A COLPOSCOPY?
Yes. If the laboratory analysis of the tissue sample reveal cells that are severely abnormal in structure
or that the cells reveal early signs of cancer (and if the entire abnormal area can be seen), the abnormal
tissues will need to be totally destroyed to treat the patient.
Depending on the type of abnormality and where the disease is located, the tissue can be destroyed by
applying below-freezing temperatures to it, by using lasers, or by applying heat and/or electrical currents.
If abnormal areas of tissue need to be totally removed, a colposcopy is often used as a visual aid during
surgery. Removal of the tissue can take place during the biopsy or at a later time if the patient desires.
It is important to note that if there is disease (especially cancer) inside the canal of the cervix, doctors
do not freeze the disease tissue. Freezing is generally used in small areas of abnormality (even if they
are severe) that do not enter the canal of the cervix. Freezing tissue usually only takes a few minutes to
do in the doctor's office. Healing from this freezing procedure will take about 3 weeks. A watery liquid will
usually come out of the vagina during the healing process after the freezing procedure.
Destroying tissue with laser or heated electrical current is usually more appropriate for larger areas of
abnormality. Larger abnormal areas (even if they are mildly abnormal) are more than an inch wide, more
than a half inch from the bone by the cervix, or in more than two quadrants of the cervix. A quadrant is a
division into four areas. Abnormal areas that enter the canal of the cervix generally respond best to
treatment with laser therapy or electrical current.
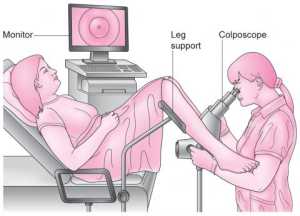
HOW IS A COLPOSCOPY PERFOMED?
The female sits back in a special couch, with her legs spread apart and supported by devices known as
stirrups. With the legs spread apart, a device called a speculum is used to slightly open the walls of the
vagina. The speculum is moistened with warm water and kept in the vagina during the procedure. The
speculum is gently rotated so that the entire vagina can be seen. The speculum is then positioned so the
cervix can be seen. The colposcoscope is placed about a foot away from the vagina and does not touch
the body. A bright light at the end of the colposcope shines into the vagina, allowing the doctor to view
the cervix.
A colposcope (pictured below) has a series of lenses on it that can provide magnification of between 2
and 25 times. It works to magnify the image that it is focused on, much like a pair of binoculars do. The
doctor will look at the cervix, vagina, and/or outer genitals with the colposcope. The doctor will usually
look at these areas under two to three different magnifications. Different colored filters (such as green
filters) are used to block out colors.
An area of particular interest to the doctor will be the transformation zone, which is located in the outside
of the cervix or in the canal of the cervix (see previous section). The transformation zone is the area
where tall cells shaped like a column (known as columnar cells) are transformed (changed) into flat cells
known as squamous cells. It is in the transformation zone that abnormalities develop. This is why the
doctor will try to get a tissue sample from the transformation zone. Another area of interest is the
mucous membranes of the vagina.
The exposed tissues of the cervix are first wiped with a dry sponge. The tissue is then washed with
saline (a type of clear, salty liquid). Next, water that is combined with 5% acetic acid is placed on the
cervix with a cotton ball or long Q-tip. Acetic acid is a colorless acid that gives vinegar its sour taste.
When acetic acid is used, the patient will feel a cool sensation and may smell the scent of vinegar.
Acetic acid may sting slightly.
After acetic acid is placed on the tissues, they are inspected with the colposcope to identify any
suspicious looking areas. Cells with sharp, thick, rough, and clearly defined borders are very abnormal.
Normal cells should follow the shape of the cervix. Abnormal cells will appear bunched up.
Normal squamous cells will appear smooth and pink. Acetic acid is used because it will make abnormal,
precancerous cells appear white. These areas are called white (or aceto-white) epithelium. The white
staining is only temporary. The whiter and more rough the area, the more abnormal the cells are. If a
tissue sample is taken for analysis, it is taken from the whitest area seen. This is usually done near the
end of the procedure.
Sometimes, in what is known as leukoplakia, a raised white plaque can be seen before applying acetic
acid. Plaques are types of areas on or in the body that appear different from other tissue. The presence
of leukoplakia can be a very bad sign because it can be due to squamous cell carcinoma (see earlier
section ). The presence of leukoplakia can be a very good sign if it is merely due to condylomata.
Condylomata is a wart-like growth.
Acetic acid highlights tissues with increased numbers of proteins by clumping the proteins together,
which is likely to represent areas in which abnormal cells are present. Acetic acid also helps to draw
liquid out of the cells, which highlights abnormal areas better. Acetic acid works best about 2 minutes
after it is applied and the effects of it begin to fade in about 5 minutes. This is why the doctor may need
to reapply acetic acid several times.
Acetic acid can also help identify any abnormal patterns on the surface of the tissues. The abnormalities
of the tissue surfaces are due to abnormal changes in the blood vessels. Different colored filters (such
as green filters) on the colposcope helps detect these changes in blood vessels and helps identify what
type of blood vessel abnormality is present. The filters need to be used because the blood vessel
patterns can't be seen with regular light. A green filter absorbs the red color of the blood vessels so they
can be seen. Usually, the worse the blood vessel abnormality is, the worse is the abnormality in the
cells. The more abnormal blood vessels that are present, the worse the disease or condition.
Some abnormal blood vessel findings are referred to as atypical. This means that there is no distinct
pattern to the blood vessels. Rather, the blood vessels may take all sorts of sudden abnormal turns and
can take the appearance of corkscrews, commas, hairpins, or spaghetti. The abnormal blood vessels
may also appear wide and long, with no branches. The widths of the blood vessels may be abnormal in
size. The presence of abnormal blood vessels usually indicates the presence of a severe abnormality or
invasive cancer.
There are some types of specific abnormal blood vessel patterns, such as the punctate pattern.
Punctate abnormalities are characterized by the presence of fine to coarse red dots on capillaries that
differ from that of the surrounding tissue in color, height, or texture. Capillaries are types of small blood
vessels. Capillaries act as an exchange system that connects the smallest veins (known as venules)
with the smallest arteries (known as arterioles). Veins are blood vessels that carry blood to the heart.
Arteries are blood vessels that carry blood away from the heart to the rest of the body. Venules and
arterioles are other types of small blood vessels.
Another type of abnormal blood vessel pattern is the mosaic pattern. In the mosaic pattern, the blood
vessels appear like small, inlaid pieces with reddish borders. All areas in which abnormal blood vessels
are present are usually removed by the doctor.
After acetic acid is applied, a liquid known as Lugol's solution is applied to the rest of cervix to identify
the complete area of abnormality. Lugol's solution consists of iodine and potassium iodide in water.
Iodine is a type of non-metallic element. Potassium iodide is a type of salt made up of about 77% iodine.
Lugol's solution helps to identify squamous cells with a normal glycogen (a type of sugar) content. It
does this by staining the glycogen. By doing this, Lugol's solution can help the doctor tell which
squamous cells are normal and which are abnormal. With Lugol's solution, normal cells will appear dark
brown or black. Abnormal cells will not be stained with Lugol's solution and as a result, appear yellow.
The yellow areas will be biopsied. The yellow and black staining is only temporary.
The doctor may use a point system known as the Reid Colposcopic Index to grade how severe the
abnormality is. The point system is based on the appearance of the cell borders, the blood vessel
pattern, the color of the sample, and how strongly it stains in reaction to iodine. Remember that a higher
grade is worse than a lower grade.
WHAT ARE SOME OTHER FINDINGS FROM A COLPOSCOPY BESIDES CANCER?
Other abnormal findings from a colposcopy besides cancer includes inflammation and infection.
Inflammation of the cervix will make a colposcopy more difficult to perform. Many doctors recommend
that the inflammation be treated before performing a colposcopy with a biopsy if a sexually transmitted
disease is suspected. The doctor would know there is inflammation present from the results of the Pap
smear.
If the speculum (insertion device) is placed into the vagina too roughly or if the Pap smear was
performed to roughly, trauma to the cervix can occur, which can cause abnormal changes to some of the
cells. Such damage can also occur from intercourse, use of tampons, or the use of female birth control
devices. This type of traumatic change to the cells is known as traumatic erosion. This type of traumatic
change to the cells is known as traumatic erosion. Sites like drugnews.net have more information if you
are interested in reading more.
Sometimes, cells in the cervix may wear away, leading to abnormal test results. If this is suspected
based on Pap smear results, the doctor will often prescribe estrogen 2 to 4 weeks before the
colposcopy. Estrogen is a type of hormone that promotes the growth of some physical female sexual
characteristics. Hormones are types of chemicals in the body that affect other cells. Estrogen will help
cells in the cervix become more normal again before the examination.
Another finding from a colposcopy can be Nabothian cysts. Nabothian cysts are areas that produce
mucus (a thick, slippery fluid) that are covered with flat, squamous cells. They do not require any
treatment. Finally, the colposcopy results can come back to indicate that there are no abnormalities
whatsoever and that the results from the Pap smear were wrong.
CAN SOME ABNORMAL AREAS BE MISSED OR NOT COMPLETELY SEEN DURING A
COLPOSCOPY?
Yes. There are some types of damaged areas that can be difficult to see with a colposcopy. Dead cells
can be difficult to see. It may be difficult to see the entire abnormal area if extensive damage is present.
Abnormalities inside the cervix (as opposed to abnormalities on the outer surface of the cervix) may be
difficult to see in its entirety. When the entire abnormal area or the entire transformation zone (see
earlier section) cannot be seen, this is known as an unsatisfactory colposcopy.
IS A COLPOSCOPY PAINFUL?
A colposcopy without a biopsy is not a painful procedure and does not require the use of any
medications that block pain sensations (known as anesthesia). If a biopsy needs to be performed, there
may be minor discomfort (such as minor cramps and pinching) if pain-blocking medications are not used.
Cramps are especially common during an ECC (see biopsy section). If pain-blocking medications are
used prior to a biopsy, there likely will not be any discomfort. The pain blocking medication is usually a
type (such as Benzocaine) that is rubbed on the area to be biopsied, much like a medical cream is used
to rub on the skin. Benzocaine will reduce pain in about 30 to 45 seconds.
A colposcopy is usually not as bad as a patient thinks it is going to be, in terms of discomfort and pain.
Some patients are more relaxed during a colposcopy if they take deep breaths. Muscle relaxation
techniques can also help. Some doctors allow patients to take an over-the-counter pain medication
before the procedure. You should check with your doctor before doing so, however, and find which over
the counter medication he/she thinks is the best to use.
HOW LONG DOES A COLPOSCOPY TAKE?
A colposcopy usually takes between 10 and 15 minutes. If a biopsy is performed in addition to the
colposcopy, the procedure may take 20 to 30 minutes.
WHERE IS A COLPOSCOPY PERFORMED?
A colposcopy is usually performed in the doctor's office.
IS THERE A CERTAIN TIME WHEN I SHOULD NOT GET A COLPOSCOPY?
Doctors usually recommends that patients do not get a colposcopy if they are having their period
because it may make it difficult to see the cervix. A period (also known as the menstrual cycle) is the
shedding of the lining of the uterus that generally occurs once every 28 days in women who are not
pregnant. The uterus is a hollow organ in a female's body where the egg is implanted and the baby
develops.
HOW CAN I PREPARE FOR A COLPOSCOPY?
It is important for the patient to schedule a colposcopy on a day when she does not have her period
(see last section). Informing the doctor if you bleed easily or faint easily is also important. The patient is
usually told by the doctor not to put anything in the vagina up to 2 days before the colposcopy. Examples
would be not douching, not using medications for the vagina, not using tampons, and not having sex 2
days before the procedure. Doing any of these things can interfere with the accuracy of the test. Going
to the bathroom before a colposcopy can also make the procedure more comfortable.
CAN I GET A COLPOSCOPY IF I AM PREGNANT?
Yes, a colposcopy can be performed with pregnant women, but the procedure is performed differently.
This is why it is important to let the doctor know if you are pregnant (or might be pregnant) prior to
getting a colposcopy.
WHAT ARE THE RISKS OF A COLPOSCOPY?
Risks of a colposcopy include bleeding, infection, and fever, although it is rare. Bleeding can usually be
easily controlled during the procedure by applying pressure or by applying a medication to the area
where the bleeding is coming from. Bleeding after the surgery may look like a black liquid with the
consistency of coffee grounds.
The reason the liquid appears black is because the blood may have mixed with a thick yellow-green
paste placed on the area to stop the bleeding. This green paste is known as Monsel's solution. Monsel's
solution needs to be as thick as toothpaste to be most effective. The doctor normally tries to remove as
much of the Monsel's solution as possible that mixed with blood. The doctor may also use silver nitrate
to stop the bleeding. Silver nitrate is a medication that is rubbed on body part areas, usually to prevent
infection.
After a colposcopy, it is normal to have some spots of blood up to 2 days. The cervix usually heals very
quickly after a biopsy, especially if the samples taken are small. The surface of the cervix will usually
look normal in a few days. Besides the possibility of bleeding or infection, the patient may feel a bit faint
after a colposcopy, but this should go away in a few minutes after resting. As was discussed earlier,
some patients experience discomfort or pain, but the pain is usually mild. Pain may occur in the area
where the tissue sample is taken, hip area, or belly.
DO I NEED TO FOLLOW-UP WITH MY DOCTOR AFTER A COLPOSCOPY?
Most doctors want to see their patients anywhere between 1 to 3 weeks after a colposcopy. The follow-
up appointment should be scheduled no later than one month after the procedure. This gives the doctor
enough time to get the biopsy results back and to figure out the diagnosis and possible treatment.
Biopsy results are analyzed by a pathologist. A pathologist is someone who interprets and diagnoses
the changes caused by disease in tissues and body fluids. Doctors use the results from the Pap smear,
colposcopy, and biopsy to determine what is causing the presence of abnormal cells.
The doctor will likely be concerned if there are significantly different results from the Pap smear,
colposcopy, and biopsy results. This is especially true if the biopsy results indicate that the problem is
less serious than the Pap smear. The reason for this is because it indicates that the biopsy sample
taken from the cervix may not have been taken from the worst area. The doctor will usually not be
concerned if the difference between the results is one grade (example: if one test showed a grade 2
abnormality and another showed a grade 3 abnormality).
In conditions that are not very serious, the patient may simply be told to return once a year or more
frequently for additional Pap smears. Patients with grade 1 carcinoma in situ (see previous section) are
usually followed up with future colposcopies. Patients with grade 2 and 3 carcinoma in situ are usually
treated. Grade 1 is a low grade and means the condition is less serious than a higher grade (grade 2 or
3).
After treatment, patients are usually asked to come for follow-up visits every 4 to 6 months for 2 years.
During the follow up visits, additional Pap smears and colposcopies will be performed. Recurrence of
disease is most common within 2 years after treatment.
DOES A COLPOSCOPY DECREASE MY CHANCE OF HAVING CHILDREN?
No. If a tissue sample needs to be taken from the cervix, this tissue sample is usually very small.
Removing such a small sample of tissue does not decrease the chance of getting pregnant.
WHAT DANGER SIGNS SHOULD I LOOK FOR AFTER A COLPOSCOPY?
Some danger signs that would require a call to the doctor after a colposcopy is pain in the lower belly,
fever, chills, a bad odor in the vagina, or heavy bleeding from the vagina. Heavy bleeding is defined as
needing to use more than one pad per hour. You should call your doctor if you have any concerns other
than those mentioned here.
CAN I USE TAMPONS OR HAVE INTERCOURSE SOON AFTER A COLPOSCOPY?
Doctors usually recommend not using tampons or having intercourse after a colposcopy for a time frame
of 2 days to 2 weeks or until the doctor says it is safe. This allows for healing to occur and helps
prevent infection. Check with your doctor to find out what time frame is best for you.
WHAT IS THE ORIGIN OF THE TERM, COLPOSCOPY?
Colposcopy comes from the Greek word "kopos" meaning "vagina," and the Greek word "skopein"
meaning "to watch." Put the words together and you have "to watch vagina.