
MedFriendly®

Diabetes Mellitus
Diabetes mellitus (often abbreviated as DM)
is a complex, long-term disorder in which
the body is not able to effectively use a
natural chemical called insulin. Insulin's
main job is to quickly absorb glucose (a type
of sugar) from the blood into cells for their
energy needs and into the fat and liver (a
large organ that performs many chemical
tasks) cells for storage. A cell is the
smallest, most basic unit of life, that is
capable of existing by itself.
FEATURED BOOK: The Eat to Live Plan
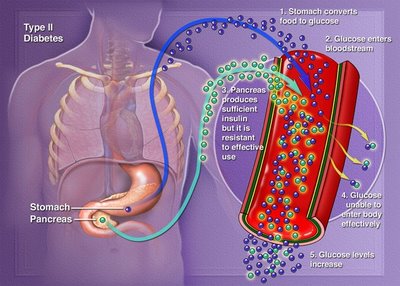
Visual diagram of Type II diabetes mellitus.
Without enough insulin to help absorb glucose, the sugar levels in the blood get too
high and glucose cannot be used effectively as an energy source. Because of this
problem, other sources in the body besides glucose need to be used for energy.
Using these additional sources for energy can lead to the buildup of toxic substances
in the body. The buildup of such toxic substances can lead to many types of
complications that are discussed in sections below.
WHY CAN'T PEOPLE WITH DIABETES MELLITUS EFFECTIVELY USE INSULIN?
There are several possible reasons why the body cannot effectively use insulin. One is
because cells (known as beta cells) in the pancreas (a long organ in the back of the
belly) fail to produce enough insulin. Worse, the beta cells in the pancreas may not
produce any insulin at all. In some cases, the body produces insulin, but cannot
effectively use it because the body resists its effects or is not sensitive to it.
WHAT ARE SOME MORE DETAILS ON HOW INSULIN
WORKS?
Insulin is normally released from the pancreas when the body
detects a rise of glucose in the blood. This usually happens a few
minutes after every meal. Insulin normally helps store glucose and
amino acids for the energy needs of cells, such as muscle cells.
Amino acids are a group of chemical substances that form
proteins. When insulin stores glucose in the liver, it changes it to a
type of carbohydrate known as glycogen. Carbohydrates are a
group of substances present in certain types of foods (such as
sugar) that provides the body with energy.
Insulin also helps prevent the formation of glucose from substances that are not carbohydrates, such
as proteins.
Since insulin helps store glucose, it helps the body tolerate glucose. Glucose tolerance is said to be
normal if a rise in glucose causes a release of insulin, which takes glucose into cells. In diabetes
mellitus, the main problem is that glucose tolerance is impaired to the point that it threatens and impairs
health.
WHAT ARE SIGNS AND SYMPTOMS OF DIABETES MELLITUS?
and symptoms of Type I diabetes develop quicker and become more severe than those of Type II
diabetes. However, the symptoms of Type II diabetes may not be noticed until a regular medical
checkup. The more severe the diabetes is, the more sugar is in the blood and the longer high blood
sugar levels last.
The high amount of sugar in the blood means that more urine is needed to carry it out of the body. As a
result, people with diabetes usually experience a strong urge to urinate, high amounts of urination, and
constant thirst. The strong urge to pee can occur at night and lead to low amounts of sleep. A high
amount of urination also leads to high amounts of water and electrolyte loss. Electrolytes are chemical
substances that are able to conduct electricity after they are melted or dissolved in water.
For people with diabetes mellitus, the urine smells sweet because the extra sugar comes out in the
urine flow. Weakness and tiredness occur because the cells in the body are not able to store or use the
sugar that they need for energy. Thus, the body is being starved of one its main energy sources. The
body still gets some energy, however, from breaking down stored fat. The breaking down of stored fat,
in turn, leads to weight loss.
Although people with diabetes mellitus can break down stored fat for energy, the body has a difficult
time doing so. People with diabetes mellitus also have a difficult time breaking down proteins. The
difficulty in breaking down fats, especially when the body does not produce insulin, can lead to the
production of acids and poisonous chemical substances called ketones. This condition is known as
ketoacidosis. Ketoacidosis is a medical emergency because it can cause coma, severe loss of body
fluids, and even death. A coma is a state of deep unconsciousness in which there are no voluntary
movements, no responses to pain, and no verbal speech. The signs and symptoms of ketoacidosis are
nausea, vomiting, abdominal pain, confusion, deep breathing, and foul-smelling breath. The foul-
smelling breath smells like nail polish remover.
Emergency treatment for ketoacidosis includes giving the person fluids to correct for fluid loss and to
bring back a normal chemical balance in the blood. Insulin injections are also given to allow cells to
better absorb glucose from the blood. Ketoacidosis can occur in people with Type I and Type II
diabetes. The difficulty with breaking down fats is especially true for people with Type I diabetes (see
two sections down for a description) if they miss several doses of insulin or develop another disease.
The reason for this is that developing another disease increases the body's use of insulin.
Other symptoms of diabetes mellitus are blurry vision, increased hunger, boils, as well as tingling and
loss of sensation in the feet and hands. Boils are inflamed, pus-filled areas of the skin. Pus is a yellow
or green creamy substance sometimes found at the site of infections.
WHAT ARE OTHER PROBLEMS AND COMPLICATIONS ASSOCIATED WITH DIABETES
MELLITUS?
Many people with diabetes mellitus eventually develop complications, especially if it is not controlled
well. Even if the diabetes is controlled well, complications can still occur. The good news is that short-
term complications can be easy to fix and that proper treatment of diabetes mellitus usually delays
complications. The bad news is that long-term complications are difficult to control and can cause
someone to die earlier than normal. Keep in mind as you read this section that there are some
individuals who have had diabetes mellitus for over 50 years and have experienced few complications.
A very common short-term complication of diabetes mellitus is hypoglycemia (abnormally low blood
sugar levels). This complication can occur during treatment if the amount of food eaten and the amount
of insulin taken are not balanced properly. Hypoglycemia is more common in people with Type I
diabetes but can occur in people with Type II diabetes who take sulfonylurea drugs. Sulfonyurea drugs
increase the production of insulin from cells in the pancreas. If untreated, hypoglycemia can cause
seizures, which are involuntary muscle movements and/or decreased awareness of the environment
due to overexcitement of nerve cells in the brain. Ketoacidosis (described in the section above) is an
example of a short-term complication of diabetes.
High levels of sugar in the blood make it more difficult for the body to fight against infections. This can
lead to infections of the urinary tract, which is the part of the body that deals with the formation and
excretion of urine. To excrete means to release from the body as waste. Skin infections can also result,
as can vaginal yeast infections (a type of infection of the female reproductive organ).
Small blood vessels throughout the body get damaged as a result of diabetes. Eye problems can
develop as a complication, such as retinopathy (also known as diabetic retinopathy), which is damage
to the retina and the blood vessels that serve it. The retina is an area at the back of the eye that is
sensitive to light. Blood vessels are tube-shaped structures that carry blood to and from the heart. Both
large and small blood vessels also start to break down quicker in people with diabetes mellitus. Blood
may also have a difficult time moving throughout the body as a result of diabetes mellitus.
Another complication is peripheral neuropathy (also known as diabetic neuropathy), which is damage to
nerve fibers outside of the brain or spine. Peripheral neuropathy can cause a gradual loss of sensation
starting at the hands and feet, which sometimes moves up the arms and legs. Loss of feeling and poor
blood circulation makes the body more susceptible to ulcers (open sores) and gangrene (tissue death
due to poor blood supply or infection of a wound). Peripheral neuropathy can also cause dizziness
when standing up as well as impotence in men. Impotence is an inability to maintain an erect penis.
Kidney damage can occur as a complication of diabetes mellitus, which can lead to kidney failure. The
kidneys are two organs located on each side of the spine, behind the stomach. The kidneys filter
(remove) wastes from the blood. The kidney damage may need to be treated by a kidney transplant or
dialysis. Dialysis is a technique in which one is hooked up to a machine that performs the functions of
the kidneys, removing wastes and extra water from the blood.
Another complication of diabetes mellitus is a higher risk for atherosclerosis, which is a narrowing of
arteries caused by a buildup of fatty substances (blood vessels that carry blood away from the heart).
Atherosclerosis can cause damage to large blood vessels, which is a major cause of stroke and
coronary artery disease. A stroke is a burst artery (a type of blood vessel that carries blood away from
the heart) or a blockage of an artery in the brain. Coronary artery disease is a narrowing of coronary
arteries, which supply the heart with blood. The narrowing of coronary arteries causes heart damage.
People with diabetes also have a greater chance to have increased levels of cholesterol, which can
speed up the development of atherosclerosis. Cholesterol is a waxy, fatty substance found only in
animal tissues.
High blood pressure, other heart disorders, and cataracts are additional complications associated with
diabetes mellitus. Cataracts is a darkening of the lens in the eye. The lens is an organ located between
the colored part of the eye, that bends light as it enters the eye.
A very important issue for people with diabetes mellitus to be concerned about is good foot care. This is
because one complication of diabetes mellitus is ulcers (open sores) on the feet. In severe cases,
ulcers can develop into gangrene. Gangrene is death of a tissue, usually due to a loss of blood supply.
If a foot sore develops, you should see the doctor immediately.
With good foot care, ulcers and infections can usually be prevented. Good foot care involves inspecting
the feet and washing and drying the feet carefully. If the skin on the feet is dry, it is recommended to
use a moisturizer to keep them moist. Good foot care also involves wearing comfortable shoes, not
walking barefoot, cutting toenails straight across, and visiting the foot doctor regularly.
ARE THERE DIFFERENT TYPES OF DIABETES MELLITUS?
Yes, there are four main types of diabetes mellitus. These types of diabetes have been listed by the
Expert Committee on the Diagnosis and Classification of Diabetes Mellitus of the American Diabetes
Association. These four types of diabetes mellitus are:
1. TYPE I DIABETES: In Type I diabetes, the cells (beta cells) in the pancreas that form and release
insulin (see above) are destroyed. The destruction of the cells that form and release insulin is probably
due to the body's response in fighting against a virus infection. In other words, the body responds to the
virus by attacking the cells that make insulin. As a result, little or no insulin is produced or released, and
there is not enough of it in the body. Type I diabetes usually first appears in people under age 35 and
most commonly in people between the ages of 10 and 16. Type I diabetes is more severe than Type II
diabetes and develops rapidly, even in children.
Type I diabetes was previously known as insulin-dependent diabetes mellitus (IDDM) because people
with this condition must inject themselves with insulin one to four times a day. The injection of insulin
helps prevent many of the problems and complications mentioned above, such as ketoacidosis, which
is an abnormal buildup of substances discussed in the previous section.
People with Type I diabetes are more prone than people with Type II diabetes to develop a condition
called ketosis. Ketosis is an abnormal buildup of substances known as ketones, which is caused by the
break down of too many fats. Ketosis can lead to the development of ketoacidosis. Ketosis and
ketoacidosis both involve a buildup of ketones. However, ketosis does not involve increased acid levels
like ketoacidosis does. See the section on signs and symptoms of diabetes to read more about
ketoacidosis. Type I diabetes is also known as juvenile diabetes, juvenile-onset diabetes, brittle
diabetes, ketosis-prone diabetes, immune-mediated diabetes, and idiopathic diabetes.
2. TYPE II DIABETES: In Type II diabetes, insulin is produced, but the cells in the body (particularly
those outside the brain and spine) resist its effects, especially when the person is overweight. Although
insulin is produced in Type II diabetes, typically not enough of it is made. Unlike Type I diabetes, Type II
diabetes develops slowly and gradually. In most cases, insulin-replacement injections are not needed.
Instead, Type II diabetes is treated with changing the diet, controlling weight, and taking medications by
mouth to control the condition.
Type II diabetes usually starts slowly, goes unnoticed for many years, and is generally discovered
during a routine medical examination. Type II diabetes typically occurs in people over 40, unlike people
with Type I diabetes. People with Type II diabetes mellitus do not tend to develop ketosis but it can
develop under stress. Type II diabetes was previously known as non-insulin-dependent diabetes
mellitus (NIDDM), ketosis-resistant diabetes, stable diabetes, adult-onset diabetes, and maturity-onset
diabetes. Both Type I and Type II diabetes mellitus are known as primary diabetes mellitus.
3. GESTATIONAL DIABETES: In gestational diabetes, women develop intolerance to glucose during
pregnancy. This intolerance is usually first recognized during the time between the 28th week of
pregnancy and birth. After giving birth, the levels of glucose usually become normal again, but may
remain impaired or develop into diabetes mellitus. Gestational diabetes occurs in 1% to 4% of all
pregnancies. Of these, 40 to 60% will develop diabetes mellitus within 15 years. Women with
gestational diabetes are often treated with insulin. Gestational diabetes is also known as asymptomatic
diabetes, subclinical diabetes, and latent diabetes.
4. OTHER SPECIFIC TYPES: There are many different possible causes of diabetes mellitus that are
not classified as Type I, Type II, or gestational. One such cause is drugs or chemicals that cause the
cells that release insulin to function improperly. In such cases, not enough insulin is formed and
released. Changes in hormones can also cause diabetes mellitus. Hormones are natural chemicals
produced by the body and released into the blood that have a specific effect on tissues in the body.
Any disease or process that negatively affects the pancreas (a long organ in the back of the belly that
makes insulin) can lead to diabetes. Such cases are known as secondary diabetes or pancreatic
diabetes. Examples of problems that can negatively affect the pancreas are wounds to the pancreas,
partial or total removal of the pancreas, and inflammation of the pancreas. Tumors (tissues that grow
more rapidly than normal) in the pancreas can also lead to diabetes mellitus, as can hemochromatosis.
Hemochromatosis is an inherited disease in which too much iron from the diet is absorbed. The iron
accumulates in the pancreas and other organs, leading to problems.
Genetic abnormalities may also play a role in the development of diabetes mellitus. This means that
there is something abnormal that is inherited from one's parents that lead to the problem. One example
would be abnormal change in cells known as insulin receptors. Picture an insulin receptor as a lock on
a door and insulin as the key. In order for insulin to work properly, it needs to fit correctly into the lock
(insulin receptor). But if the lock has changed shape, insulin (the key) can no longer fit into it, and thus
it cannot work the way it is supposed to.
People with such a genetic problem tend to have severe diabetes, and too much sugar and insulin in
the body. There is too much insulin in the body because it cannot fit into the receptors and there is too
much sugar because the insulin cannot function properly to take the sugar away.
Another possible genetic cause of diabetes mellitus is an inherited defect in the cells that produce
insulin. People with such a defect may have an inability to change proinsulin into insulin. Proinsulin is a
natural protein that is normally used to make insulin. Such people may also produce an abnormal type
of insulin that does not work properly. They may also have abnormalities in glucokinase, which is a type
of protein that speeds up chemical reactions involving a form of glucose. Diabetes in which there is a
genetic defect in the cells that produce insulin is known as maturity onset diabetes of the young
(MODY).
A rare inherited disease, called lipoatrophic diabetes is characterized by Type I diabetes, loss of body
fat, wasting away of muscles, fast metabolism, and other signs and symptoms. Metabolism is the
chemical actions in cells that release energy from nutrients or use energy to create other substances.
Infections, such as adenovirus, cytomegalovirus, and coxsackievirus B, can lead to diabetes by
destroying the cells that make insulin. Any diseases or dysfunction involving an endocrine gland can
lead to diabetes mellitus, by decreasing the amount of insulin that is produced. An endocrine gland is a
type of organ (such as the pancreas) that releases hormones (types of natural chemicals) into the
blood or lymph nodes. Lymph nodes are small egg shaped structures in the body that help fight against
infection.
There are few known conditions of some rather uncommon forms of diabetes mellitus (that do not
qualify as Type I, 2, or gestational diabetes), in which the body produces substances to fight against
insulin. Some people who have developed this condition have received a medication called interferon-
alpha, which is used to fight against forms of cancer. Cancer is a group of diseases in which symptoms
are due to an abnormal and excessive growth of cells in one of the body organs or tissues. Some other
people who have developed this uncommon form of diabetes have had a condition known as stiff man
syndrome, in which there is no known cause and the muscles alternate between being stiff and loose
over time.
WHAT ABOUT PEOPLE WITH IMPAIRED GLUCOSE TOLERANCE?
There are a group of people whose levels of glucose in the blood are abnormally high, but not high
enough to be classified as diabetic. This group is called the impaired glucose tolerance group, and
many in this group are obese (very overweight). In this group, 10% to 25% will develop Type II diabetes
within 10 years.
WHAT CAUSES DIABETES MELLITUS?
In Type I diabetes, the body's defense system (known as the immune system) destroys cells (beta
cells) in the pancreas that form and release insulin. The destruction of the cells that form and release
insulin is probably due to the body's response in fighting against a virus infection. In other words, the
body responds to the virus by attacking the cells that make insulin. As a result, little or no insulin is
produced or released, and there is not enough of it in the body. In some cases, the destruction of the
insulin producing cells is caused by inflammation of the pancreas (a long organ in the back of the belly).
Diabetes mellitus also tends to run in families. This means that the child of a parent with diabetes has a
higher chance of developing the same type of diabetes than a child whose parents do not have
diabetes. However, only a small percent of people who inherit the genes for Type I diabetes (insulin-
dependent) actually go on to develop the disease. Genes are units of material contained in a person's
cells that contain coded instructions as for how certain bodily characteristics (such as eye color) will
develop. All of a person's genes come from his/her parents.
So why do some people who inherit the genes for Type I diabetes go on to develop the disease while
others do not? The answer is that in many cases (but not all), Type I diabetes may occur because of
having the genes for this disease as well as having a delayed reaction to a virus that damaged the
pancreas several years earlier.
There is a subgroup of people with Type I diabetes in which the cause is not known. This is known as
idiopathic diabetes. In these individuals, the need to take insulin injections can very from time to time.
In other words, sometimes it will be necessary for them to take the insulin injections and other times it
will not.
Unlike Type I diabetes, a greater percentage of people who inherit the genes for Type II diabetes (non-
insulin-dependent) actually go on to develop the disease. Thus, there appears to be a strong genetic
component to Type II diabetes. However, it is generally overweight people who go on to develop this
form of diabetes. Obese (very overweight) people are particularly likely to develop the Type II form,
rather than the Type I form. Such people tend to have very large bellies.
In societies where people are making a lot of money, there are more and more cases of Type II
diabetes mellitus. Why? The people living in such societies have more money and can buy more food.
This means that these people eat more, which leads to an increase in the number of overweight people
and thus, an increase in the amount of people with Type II diabetes mellitus.
People with Type II diabetes also tend to have high amounts of fat and fatty proteins in their blood.
Having a lifestyle in which one does not exercise much and sits around most of the day is another risk
factor for developing diabetes. Another risk factor is having a diet that is high in fat a low in dietary fiber.
Dietary fiber is a term for chemical substances in the cells of plants that cannot be digested by the
human body.
Other factors that can increase the chance of developing diabetes mellitus include: pregnancy, high
blood pressure, infections, and certain illnesses. Illnesses that can cause diabetes mellitus include
pancreatitis (inflammation of the pancreas) and thyrotoxicosis (a poisonous condition that results from
an overactive thyroid gland). The thyroid gland is a butterfly-shaped organ located in front of the neck
that produces a natural chemical known as hormones that affect virtually every cell in the body and
many functions such as heart rate, energy level, and skin condition.
Certain drugs can also lead to diabetes mellitus, such as diurectics, which increase the amount of
water flowing into the urine. Benzothiazides (also known as thiazides), which are drugs that reduce
high blood pressure and increase the amount of water flowing into the urine, can also lead to diabetes
mellitus.
Corticosteroids can also lead to diabetes because they work against the actions of insulin.
Corticosteroids are a group of drugs that act similarly to a natural chemical in the body known as
corticosteroid hormone. Corticosteroid hormones control the body's use of nutrients and the amount of
water and salts in the urine. Even excess levels of natural corticosteroid hormones can cause Type II
diabetes mellitus. Diabetes caused by corticosteroids is sometimes known as steroid diabetes.
Hormone treatments, such as growth hormone, thyroid hormone, and adrenocorticotropin hormone
(ACTH) can lead to diabetes mellitus. Hormones are natural chemical produced by the body and
released into the blood that have a specific effect on tissues in the body. Growth hormone promote
growth, ACTH promotes the release of corticosteroids (see last paragraph), and thyroid hormone helps
with metabolism. Metabolism is the chemical actions in cells that release energy from nutrients or use
energy to create other substances. Sometimes hormones are administered as medical treatment for
certain medical conditions. For example, ACTH is used to treat allergies that won't go away, various
skin disorders, and other problems.
HOW MANY PEOPLE HAVE DIABETES?
Diabetes mellitus is one of the most common long-term diseases in the United States, affecting more
than 1 out of every 20 people. Overall, it is estimated that approximately 16 million people have
diabetes in the United States. Of these, 95% are classified as Type II diabetes (non-insulin dependent).
More than 70% of these patients (those with Type II) are obese (very overweight).
Type II diabetes generally occurs in people over age 40 and affects as many as 2,000 people out of
every 100,000. In total, about 7.5 million people have Type II diabetes. By contrast, Type I diabetes
(insulin dependent) affects about 150 to 200 people out of every 100,000. In total, about 800,000
people in the U.S. have Type I diabetes.
About 2 people out of every 1000 persons have Type I (insulin dependent) diabetes by age 20. In
addition, 75% of people who develop Type I diabetes get it by age 30, but it can occur all the way up to
the 100s. Most people with Type I diabetes have symptoms before age 25. About 650,000 new cases
of diabetes mellitus are diagnosed each year in the United States.
HOW IS DIABETES MELLITUS DIAGNOSED?
If a doctor believes that a patient has diabetes mellitus, he/she can confirm this by testing the amount
of glucose (a type of sugar) that is present in the urine. If the level of glucose is too high, diabetes is
suspected. The doctor can further confirm that diabetes is present by sending the patient for a blood
test and finding that the level of glucose in the body is too high. The blood test is usually done after the
person spent the night before the blood test without eating. However, the blood tests can also be taken
2 hours after a meal.
The blood may also be tested for glycosylated hemoglobin. Glycosylated hemoglobin is a substance in
red blood cells that carries oxygen and is bonded with a form of glucose and other sugars. People with
diabetes mellitus usually have higher than normal levels of glycosylated hemoglobin when gluocose
levels have been high for several weeks or months. The doctor will also ask you questions about your
medical history to try to make a diagnosis.
For more specifics on how diabetes mellitus is diagnosed, check out the American Diabetes
Association, which revised their criteria for diagnosing it in June of 1997. All of these criteria depend on
the amount of sugar that is present in the plasma (a type of fluid in the blood) of the veins. Veins are
blood vessels that carry blood to the heart. If any two tests show that the amount of glucose in the body
is at or above a certain established level on two separate days, diabetes mellitus will be diagnosed.
There are many people who have a mild form of diabetes mellitus that are unaware of it. They often do
not get diagnosed until symptoms and complications arise. See the beginning of this entry for a
description of symptoms and complications that occur in diabetes mellitus. All people who have insulin-
dependent (Type I) diabetes that do not get treatments will develop symptoms. However, only about
one out of three people with non-insulin dependent diabetes (Type II) will develop symptoms.
HOW IS DIABETES TREATED?
In treating diabetes, the goal is to help the person live longer, relieve symptoms, and prevent long-term
difficulties. In order to accomplish this, the levels of glucose and insulin in the blood need to be kept
normal, in relation to each other, without significant changes. Levels of glucose in the blood are kept
normal by keeping weight at a normal level and having a proper diet.
Diet may also be combined with exercising regularly, and/or taking insulin injections and possibly other
medications, depending on the case. Although treatment needs to be tailored to each individual,
treating Type I diabetes by only taking medications by mouth does not usually work. Treatment of
diabetes is usually lifelong.
In the 1990's medications were developed to increase the responsiveness of cells to insulin, work
against the resistance of cells to insulin, and reduce carbohydrate absorption after meals. For people
with Type I or Type II diabetes, keeping glucose at or near normal levels significantly reduces the
chances of developing many of the complications mentioned above (such as eye disease, kidney
disease, and nerve damage).
INSULIN INJECTIONS:
People with Type I diabetes inject themselves with insulin one to four times a day for long-term
survival. About 1 in 10 people treated for diabetes mellitus need to take insulin injections for life. Insulin
is a natural chemical that is produced by the pancreas. Insulin's main job is to absorb glucose (a
sugar) into cells for their energy needs and into the liver and fat cells for storage. Insulin is available in
forms that work over the short-term, long-term, and a combination of both.
The insulin that people inject into themselves comes from animals or from a human type produced by
genetic engineering (altering genes). Genes are units of material contained in a person's cells that
contain coded instructions as for how certain bodily characteristics (such as eye color) will develop.
Stress of any kind may make it necessary to change the dosages of medications used to treat
diabetes.
Insulin is commonly injected into the skin with a needle that can be thrown away after use. However,
many people prefer insulin pens, which are easier to use and easy to keep out of site. The insulin pen
has a push button on one end to release the needle that is at the other end. It also has a dose selector
dial that allows the individual to select the dose of insulin to be injected. There is also an insulin scale
on the pen so the person can see how much insulin is left. Since the insulin pen has refillable insulin
cartridges, it is useful if many injections need to be made throughout the day. The needles in an insulin
pen can be thrown away after use.
People who have diabetes that is difficult to control may use a pump that sends insulin into the body
through a tube with a smooth, unsharpened point that is injected into the skin. This device, known as
an insulin pump, sends insulin into the body throughout the day. The insulin pump, which is refillable,
can easily be carried around because it clips onto a belt.
After about age 10, children can be taught how to inject themselves with insulin if they have diabetes.
For children, an easy place to inject the insulin is in the thigh. Insulin can be injected into any fatty area
in the body, such as the upper arms or stomach, in addition to the thighs. The insulin is inserted by
sticking the needle in quickly and pushing the insulin in slowly. Doctors recommend against using
exactly the same site each time for an injection.
People who use an insulin pump need to monitor their blood glucose levels carefully and should
periodically measure their glycosylated hemoglobin. Glycosylated hemoglobin is a substance in red
blood cells that carries oxygen and is bonded with a form of glucose and other sugars. People with
diabetes mellitus usually have higher than normal levels of glycosylated hemoglobin when glucose
levels have been high for several weeks of months.
If there if too much glucose in the blood, this is known as hyperglycemia, Hyperglycemia can cause the
symptoms of untreated diabetes (see sections above). If there is too little glucose in the blood, this is
known as hypoglycemia. Hypoglycemia can lead to confusion, weakness, sweating, dizziness,
unconsciousness, and seizures (involuntary muscle movements and/or decreased awareness of the
environment due to overexcitement of nerve cells in the brain). If glucose in the body is higher or lower
than usual, a doctor will help adjust the dose of insulin and may suggest changes in diet.
MONITORING GLUCOSE:
People with diabetes often test their own blood and urine to find out the level of glucose in it. Such
monitoring is especially important if the person exercises, plans to eat a lot, or develops another
illness. Monitoring blood glucose takes place at least once per day or more, depending on the doctor's
recommendations. Monitoring glucose in the blood is done by pricking the skin with a small needle that
is released from a springing device. Usually, the fingertip is pricked after washing and drying the
hands.
A small sample of blood is taken and spread on a strip that is covered with chemicals, which reacts
with glucose. The person waits for about a minute (or more, depending the machine) and then wipes
off any extra blood from the strip. The strip is then placed in a digital meter that instantly provides the
level of glucose in the blood sample. Many individuals who have received more than they need
through their insurance plan will often decide to sell test strips online to those who need them.
Testing the urine is somewhat easier because it only requires sticking a strip that is covered with
chemicals into a sample of urine. The urine reacts with the chemicals on the strip and turns a certain
color. The color on the strip is then compared with a color chart to determine the level of glucose in the
urine.
To prevent sugar levels from getting too low, people with Type I diabetes need to carry around some
sugar or foods containing sugar or glucose with them at all times. Since abnormally low sugar levels
can cause some very disabling problems (see above), people with Type I diabetes who drive need to
tell insurance companies and car-licensing companies about their condition.
OTHER RECOMMENDATIONS:
Because of the problems associated with Type I diabetes, people who have poor control over this
condition are sometimes warned against performing jobs that involve high risk activities. Such activities
include flying, racecar driving, working in high places, and any other risky activities.
It is helpful for people with diabetes to carry or wear information that states that they have diabetes.
This information is important for health care providers to know in case of an emergency. It is also
helpful for the individual to be educated about diabetes, which can be accomplished through self-help
groups.
People with Type I diabetes may be asked to exercise regularly and must follow a diet in which foods
and beverages containing carbohydrates are consumed at a normal level and meals are spaced
throughout the day according to a consistent timetable. By controlling the level of carbohydrates that
are consumed, major changes in glucose levels in the blood can be avoided. This is because glucose
is found in carbohydrates. People with diabetes also have difficulty breaking down carbohydrates in
their bodies. People with Type I diabetes typically measure the glucose and sugar levels in their blood
with do-it-yourself testing kits.
For people with Type II (non-insulin dependent) diabetes, sometimes the only treatment necessary is
to control diet. This is because in Type II diabetes, the pancreas is producing some insulin. As was
mentioned earlier, the diet is controlled by consuming a normal level of carbohydrates, keeping fat
intake low, and by spacing meals throughout the day. Energy should come from foods with complex
carbohydrates in them, such as bread and rice.
People with Type II diabetes should follow general guidelines for a healthy diet and should seek out
help from a dietician (dieting specialist) if necessary. The person should try to eat the same amount of
calories each day. This can be done by eating the same amount of fats, carbohydrates, and proteins
each day. By following such a diet, the level of sugar and body weight gets lowered. People with Type
II diabetes typically measure the glucose and sugar levels in their blood with do-it-yourself testing kits.
If changes in diet are not enough to lower the amount of glucose in the body, exercise has also been
shown to help. In addition, insulin injections may need to be taken and/or one or more medications
taken by mouth (known as hypoglycemic tablets or sulfonylureas) that help the pancreas to make more
insulin. If glucose levels are too high, a drug called acarbose may be given to slow the rate in which
the body absorbs glucose from the intestine, preventing changes in the blood level of glucose. The
intestine is a tube shaped structure that is part of the digestive tract. It stretches from an opening in the
stomach to the anus (rear end) and occupies most of the lower parts of the belly.
If drugs taken by mouth do not work, they may need to be injected. These medications will not work
unless the diet is also being managed in the way that was previously described. In addition, stress of
any kind may make it necessary to change the dosages of medications used to treat diabetes.
For people who need diabetes mellitus to be treated intensively, the risk of heart disease may be
increased because the body weight generally increases, as does blood pressure, and levels of fat and
cholesterol. Cholesterol is a waxy, fatty substance found only in animal tissues.
FOLLOW-UP CARE:
People with diabetes need to stay in contact with their doctors so that any complications can be found
and treated early. As a general rule, people with diabetes mellitus see their doctors every few months
(usually 4 times a year) so that problems can be detected early and treated effectively. The doctor will
usually perform an eye exam once a year, a neurological exam, test the urine for kidney disease and
will examine blood pressure, blood sugar, and the pulse. The pulse is the regular and reoccurring
widening and narrowing of an artery (a blood vessel that carries blood away from the heart) that is
caused by blood pressure.
The eye exam for people with diabetes mellitus involves examining the retina (the light sensitive area
in the back of the eye) to see if diabetes has caused it any damage. The neurological exam helps to
see if the spine and nerves in the head and brain are working properly. Some people with diabetes
prefer to see an ophthalmologist once a year. An ophthalmologist is a medical doctor that specializes
in ophthalmology, which is the science that deals with the structure, functions, and diseases of the
eye, and the diagnosis and treatment of such diseases.
WHAT HAPPENS IF TYPE I DIABETES MELLITUS IS NOT TREATED?
If diabetes mellitus is not treated with injections of insulin, the affected person will fall into a coma and
eventually die. A coma is a state of deep unconsciousness in which there are no voluntary movements,
no responses to pain, and no verbal speech.
CAN TYPE I DIABETES BE CURED?
Yes, but for most people diabetes mellitus is usually permanent. At the present time, the only way to
cure Type I diabetes is by removing a person's pancreas and replacing it with a donated pancreas.
This treatment option is not offered routinely because of the possibility that the person will reject the
new pancreas and because the person needs to be placed on medications (known as
immunosuppressant drugs) for the rest of his/her life to prevent or decrease the chance of this
happening.
A pancreas transplant may be done, however, if the person is scheduled to have a kidney transplant.
The kidneys are two organs located on each side of the spine, behind the stomach. The kidneys filter
(remove) wastes from the blood. An experimental treatment is being developed in which insulin-
producing cells from a normal pancreas can be taken and placed into a pancreas that is not
functioning properly.
SHOULD PEOPLE WITH DIABETES STOP SMOKING?
Yes. Smoking should stop because it greatly increases the chances of developing heart disease,
stroke, and other long-term complications. A stroke is a burst artery (a type of blood vessel that carries
blood away from the heart) or a blockage of an artery in the brain.
WHAT SHOULD EXERCISE BE LIKE FOR PEOPLE WITH DIABETES MELLITUS?
Exercise, such as walking, is important for people with diabetes mellitus because it may improve
control over diabetes. Exercise can make one feel healthy, and can reduce the risk of stroke (see
above), high blood pressure, and heart disease. It can also help reduce weight if that is needed.
People with Type I diabetes may need to monitor their blood glucose levels before, during, and after
exercise. This is because exercise can affect the body's need for insulin. During stressful exercise,
such as playing in a competitive basketball game, blood glucose levels are usually reduced. Thus,
before strenuous exercise, people with diabetes mellitus may need to eat more or adjust their insulin
levels.
WHAT TYPE OF DIET IS SUGGESTED FOR PEOPLE WITH DIABETES MELLITUS?
For some people with diabetes mellitus, a healthy diet and weight loss is enough to keep glucose
levels in the blood normal. Most doctors suggest the diet described below for people with diabetes
mellitus. Keep in mind that these are general guidelines and you should consult your doctor to see
what type of diet is most appropriate for your needs. The following is a list of parts of the diet in
alphabetical order, for people with diabetes mellitus:
ALCOHOL: Too much alcohol can lower glucose levels and cause weight gain. This is why alcohol
needs to be consumed in moderation, if it is to be consumed at all. You should talk with your doctor to
find out what levels are appropriate for you, since this depends on your body weight.
ALTERNATIVE SWEETENERS: There is no evidence to date that it is a problem for people with
diabetes to use alternative sweeteners.
CALORIES: People with diabetes mellitus need to take in enough calories to maintain a normal body
weight.
CARBOHYDRATES: Carbohydrates are a group of substances present in food (such as sugar) that
provides the body with energy. By controlling the level of carbohydrates that are consumed, major
changes in glucose levels in the blood can be avoided. This is because glucose is found in
carbohydrates. For people with diabetes mellitus, between 45% and 50% of their daily calories should
come from carbohydrates. However, this number will vary from person to person depending on the
amount of fats and proteins they consume. The diet should be high in complex carbohydrates, which
are found in foods such as rice and pasta.
People with diabetes mellitus should be consistent in the percentage of carbohydrates that are eaten
each day. Refined sugars (such as sucrose) may be consumed in modest amounts, depending on the
person's body weight and rate of metabolism. The rate of metabolism is the speed in which the body
proceeds with chemical reactions involved in distributing nutrients in the blood after food is broken
down and digested. Refined sugars are those that are purified before they are used for food.
DIETARY FIBER: People with diabetes mellitus should consume up to 40 grams of dietary fiber a day.
A gram is a very small unit of weight. For people who consume low amounts of calories, they should
have 25 grams of dietary fiber for every 1000 calories.
FAT: Usually, fat intake should be less than or equal to 30% of total calories, but it may be as high as
40%. Fats from animals should be especially limited. Of the 30% of calories from fat, 6% to 8% should
be polyunsaturated fats, 10% should be saturated fats, and monosaturated fats should make up the
rest. Cholestorol should be less than 300 milligrams per day. Cholestorol is a waxy, fatty substance
found only in animal tissues.
Saturated means to be filled up with something. In the case of fats, saturated refers to how much
hydrogen (a kind of element) is contained in it. Saturated fats are filled with hydrogen and are the most
harmful to eat. Monosaturated fat has only one gap in it where there is no hydrogen. Polyunsaturated
fat has many gaps in it where there is no hydrogen and comes mainly from plants. The levels of fats
that should be consumed for a person with diabetes mellitus will differ depending on the amount of fat
in their blood and in the rest of their body.
PROTEIN: People with diabetes mellitus usually need to have twice the levels of protein than the
average person. About 12% to 30% of total calories should come from protein. For people with kidney
disease, consuming too much protein should be avoided.
SALT: People with diabetes mellitus should have less than or equal to 3000 milligrams per day. A
milligram is one thousandth of a gram. People with special conditions such as high blood pressure
may need to have less sodium in their diet.
VITAMINS AND MINERALS: There is no evidence to date that people with diabetes need more
vitamins or minerals than people without diabetes mellitus.
WHAT IS THE OUTLOOK FOR PEOPLE WITH DIABETES MELLITUS?
Although diabetes mellitus is a serious disease, it is easier to control today due to advances in
monitoring blood sugar levels. People who monitor their condition carefully, maintain a healthy lifestyle,
and follow through with medical treatment can expect to live an otherwise normal life. People with Type
I (insulin dependent) diabetes have a normal life expectancy. People with Type II (non-insulin
dependent) diabetes has a slightly lower life expectancy than normal because many of them have
heart disorders and difficulties with blood circulation when the disorder is diagnosed. Overall, diabetes
mellitus is the 7th leading cause of death in the United States.
HOW MUCH DOES DIABETES MELLITUS COST THE NATIONAL ECONOMY?
Diabetes mellitus costs the national economy of the United States national economy over 100 billion
dollars a year.
WHAT DOES DIABETES MELLITUS HAVE IN COMMON WITH DIABETES INSIPIDUS?
Besides urinating too much and drinking a lot, diabetes mellitus does not have much in common with
diabetes insipidus. Diabetes insipidus is a much more rare condition in which a small organ in the brain
known as the pituitary gland does not produce enough of a natural chemical known as antidiuretic
hormone (ADH). Normally, ADH works to decrease the amount of water that enters the urine. However,
if there is not enough ADH, the reverse happens, and too much water enters the urine and leaves the
body.
WHAT IS THE ORIGIN OF THE TERM, DIABETES MELLITUS?
Diabetes mellitus comes from the Greek word "diabainein" meaning "to pass through," and the Latin
word "mellitus" meaning "sweetened with honey." Put the two words together and you have "to pass
through sweetened with hon