
MedFriendly®


Normal Pressure Hydrocephalus
Before discussing normal pressure hydrocephalus, it is
necessary to understand hydrocephalus and the role of
cerebrospinal fluid (abbreviated CSF). Hydrocephalus
is a condition in which there is an abnormal increase in
cerebrospinal fluid inside the head. CSF is the
cushiony fluid that protects the brain and spine and
helps distribute nutrients to these structures. CSF is
produced by openings in the brain known as ventricles.
Increased CSF causes the ventricles to become wider
because they need to expand outwards to make room
for the extra fluid.
FEATURED BOOK: Normal Pressure Hydrocephalus: Pathophysiology, Diagnosis,
CSF is produced by a cluster of blood vessels that line each of the ventricles. These
clusters of blood vessels are known as the choroid plexus. After leaving the fourth
ventricle, CSF flows around the brainstem. The brainstem is an area in the lower part of
the brain that connects it with the spinal cord. In the picture above, the fourth ventricle is
shown in the brainstem.
The CSF also flows around the cerebellum and the two halves of the brain. The
cerebellum is an area in the back, bottom part of the brain that plays an important role in
movement and coordination. In the picture above, the cerebellum is the yellow-orange
area behind the fourth ventricle.
"Where Medical Information is Easy to Understand"™
CSF then flows down the subarachnoid space,
which is a space located between two layers that
cover the brain -- the arachnoid mater and the pia
mater. The CSF then flows back up to the basal
cisterns. The basal cisterns are spaces behind the
brainstem that hold CSF. CSF is usually absorbed
by bumpy structures in the ventricles known as
arachnoid granulations, and brought out into the
bloodstream.
WHAT IS NORMAL PRESSURE
HYDROCEPHALUS?
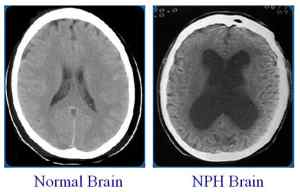
Enlarged lateral ventricles are
a classic sign of NPH.
Normal pressure hydrocephalus is a type of hydrocephalus characterized by increased cerebrospinal fluid
and a widening of the ventricles of the brain, usually without causing increased pressure inside the head.
The pressure is usually normal because the ventricles widen to make room for the extra fluid. A
consequence of this widening, however, is that the increased fluid presses against certain brain
structures, damaging or destroying them.
Although normal pressure hydrocephalus usually presents without an increase of pressure inside in the
head, increased pressure can happen if the condition goes untreated. Increased pressure on brain
structures can cause worsen the signs described below and cause significant brain damage.
HOW IS CEREBROSPINAL FLUID NORMALLY MADE AND DISTRIBUTED?
There are four ventricles (openings) in the brain that produce CSF. These ventricles are the fourth
ventricle, third ventricle, and the two lateral (side) ventricles. A picture of these ventricles is shown below:
WHAT CAUSES NORMAL PRESSURE
HYDROCEPHALUS?
Many times, the cause of normal pressure
hydrocephalus is unknown. However, the condition is
often caused by a failure of the arachnoid granulations
(see earlier section) to absorb enough of the
cerebrospinal fluid. As a result, the cerebrospinal fluid
level increases, even though it is being produced in
normal amounts.
In other cases, something is blocking the flow of
cerebrospinal fluid, causing normal pressure
hydrocephalus.
Any condition that causes a blockage of cerebrospinal fluid can lead to normal pressure hydrocephalus.
Some causes of blocked cerebrospinal fluid include a closed head injury, brain surgery, brain tumors,
and infections in the brain. Normal pressure hydrocephalus general occurs weeks after brain infections
such as meningitis. Meningitis is an inflammation of the meninges (the three outer coverings of the
brain and spinal cord). Meningitis can cause scarring to the arachnoid granulations, which help absorb
cerebrospinal fluid. If the arachnoid granulations are scarred, they will not absorb the cerebrospinal fluid
adequately.
A subarachnoid hemorrhage can also cause normal pressure hydrocephalus. A subarachnoid
hemorrhage is when bleeding occurs in the space between two of the layers that cover the brain - the
arachnoid mater and the pia mater. In the case of a subarachnoid hemorrhage, the blood is what blocks
the flow of cerebrospinal fluid. Generally, this blockage occurs in the outlets of the fourth ventricle or in
the cerebral aqueduct. The cerebral aqueduct is a narrow opening in the brain that connects the third
ventricle with the fourth ventricle, allowing cerebrospinal fluid to flow between these two areas. It can
be viewed in the picture above.
About 10-20% of patients with a subarachnoid hemorrhage will develop normal pressure hydrocephalus
that causes noticeable signs. Normal pressure hydrocephalus may take up to several months to
develop after a subarachnoid hemorrhage has occurred. Many head injuries cause subarachnoid
hemorrhages.
Although very rare, it does appear that in some cases normal pressure hydrocephalus can be inherited
(passed on through the genes of one's parents). This is still debatable, however. Genes are tiny
structures that contain coded instructions for how proteins should be constructed and how certain
bodily characteristics should develop. For example, genes control the natural color of people's eyes
and hair, and whether they will be male or female. Genes are passed on from parents to their children.
WHAT ARE RISK FACTORS FOR NORMAL PRESSURE HYDROCEPHALUS?
Risk factors for normal pressure hydrocephalus include closed head injury, brain surgery, infections in
the brain, and a subarachnoid hemorrhage (see earlier section). Other risk factors for normal pressure
hydrocephalus include high blood pressure, coronary artery disease, and diabetes mellitus. Coronary
artery disease is a narrowing of coronary arteries, which are blood vessels that supply the heart with
blood.
Diabetes mellitus is a complex, long-term disorder in which the body is not able to effectively use a
natural chemical called insulin. Insulin's main job is to quickly absorb glucose (a type of sugar) from the
blood into cells for their energy needs and into the fat and liver (a large organ that performs many
chemical tasks) cells for storage.
Another risk factor for normal pressure hydrocephalus is a low level of HDL in the blood. HDL stands for
high-density lipoprotein cholesterol. Cholesterol is a waxy, fatty substance found only in animal tissues.
HDL is called the "good cholesterol" because it helps prevent cholesterol from building up in your
arteries.
HOW IS THE PRESSURE OF CEREBROSPINAL FLUID MEASURED?
The pressure of cerebrospinal fluid is most commonly measured with a spinal tap (also known as a
lumbar puncture). A spinal tap is a procedure in which a needle is inserted into a space inside the spinal
canal for the purpose of removing some of the cerebrospinal fluid. The spinal canal is the space
between the spinal cord and the bony structure that surrounds it. It is because the pressure inside the
head is usually normal, that this condition is called normal pressure hydrocephalus.
IS THE PRESSURE OF CEREBROSPINAL FLUID ALWAYS NORMAL IN NORMAL PRESSURE
HYDROCEPHALUS?
Actually, the answer is no. The pressure of cerebrospinal fluid in normal pressure hydrocephalus can be
higher than normal in some cases, particularly in the beginning stage. After the beginning stage,
however, the pressure usually returns to normal as the ventricles enlarge to hold the increased fluid. In
some cases, increased cerebrospinal fluid pressure can occur in the middle stage of this condition.
Thus, the term normal pressure hydrocephalus is not entirely an accurate term in some cases.
WHAT ARE THE SIGNS OF NORMAL PRESSURE HYDROCEPHALUS?
There are three main signs of normal pressure hydrocephalus that usually occur gradually rather than
suddenly. These signs are difficulty walking, difficulty holding in urine, and difficulty thinking. The
difficulty walking usually presents as a slowed, shuffling walk, in which the feet appear stuck to the
ground. The person may appear unsteady when walking, may have difficulty starting to walk, may have
difficulty making turns, and may also complain of weakness in the legs.
The difficulty walking may lead to sudden falls without a loss of consciousness. Difficulty walking in
normal pressure hydrocephalus seems to be associated with increased tension in the extensor muscles
of the legs. The extensor muscles are muscles that extend (the opposite of flex) body parts). It should
be noted that some patients with normal pressure hydrocephalus only present with a difficulty walking.
In addition to difficulty holding in urine, the person may also have difficulty holding in feces. This only
occurs in rare circumstances, however. In earlier stages, patients may not lose control of their ability to
hold in urine or feces, but they may have increased urges to urinate or have bowel movements, and
may actually perform these bodily functions more often.
The thinking difficulties in normal pressure hydrocephalus are usually characterized by confusion, poor
attention, slowed thinking, and memory difficulties. The thinking difficulties can eventually progress into
a dementia. Dementia is a mental disorder characterized by a significant loss of intellectual and
cognitive abilities without impairment of perception or consciousness. It is estimated that about 5% of
all dementias are due to normal pressure hydrocephalus. If treated early enough, dementia from normal
pressure hydrocephalus can be reversible. The dementia will initially present as mild and can progress
to severe.
Patients with normal pressure hydrocephalus may have rigid muscles and tremors (uncontrollable
shaking movements). Patients with normal pressure hydrocephalus may have an abnormally weak
voice due to incoordination of the muscles that control speech.
A person with normal pressure hydrocephalus may have no observable mood. That is, they do not
appear happy or sad, but rather indifferent and withdrawn. Their facial expressions may appear to be
very restricted. They may not be very spontaneous in terms of movements or conversations, requiring
other people to act first before they speak or move. Expressive speech may be impaired in people with
normal pressure hydrocephalus.
WHAT CAUSES THE SIGNS OF NORMAL PRESSURE HYDROCEPHALUS?
The signs of normal pressure hydrocephalus are caused by distortion of the central portion of the
corona radiata, which is due to a widening of the ventricles. The corona radiata is a fan-shaped
network of fibers that weaves through the white matter of the cortex (the top, main section of the brain)
and connects with the fibers of the corpus callosum. White matter is white appearing nerve fibers in the
brain and spine that help transmit messages fast. The corpus callosum is a large band of nerve fibers in
the brain that help the two sides of the brain communicate with each other.
The nerve fibers in the corona radiata send nerve impulses to the legs and the urinary bladder, which is
why difficulty walking and difficulty controlling the urge to urinate occurs. The urinary bladder is a hollow,
muscular organ in the body that collects and temporarily holds urine until it is ready to leave the body.
Dementia results from distortion of the limbic system near the ventricles. The limbic system is an area
near the edge of the middle part of the brain that is important for proper memory functioning and for
producing emotions.
It should be noted that increased pressure from cerebrospinal fluid in enlarged ventricles applies
considerably more force against the brain than the same pressure in normal size ventricles.
HOW MANY PEOPLE DEVELOP NORMAL PRESSURE HYDROCEPHALUS?
Approximately 250,000 people in the United States develop normal pressure hydrocephalus each year.
WHO USUALLY GETS NORMAL PRESSURE HYDROCEPHALUS?
People who develop normal pressure hydrocephalus tend to be elderly individual 60 years and older.
HOW IS NORMAL PRESSURE HYDROCEPHALUS DIAGNOSED?
Unfortunately, normal pressure hydrocephalus is difficult to diagnose. One of the reasons for this is
because the tests used to get pictures of the inside of the brain (such as CT scans or MRIs) do not
show a pattern that definitively indicates that the condition is normal pressure hydrocephalus and
nothing else. CT (computerized tomography) scanning is an advanced imaging technique that uses x-
rays and computer technology to produce more clear and detailed pictures than a traditional x-ray. MRI
using very powerful magnets and computer technology.
A test known as a cisternogram may show changes of the flow of cerebrospinal fluid in the brain.
Specifically, the cisternogram scan may show that the fluid flowed back into the ventricles (openings in
the brain that produce cerebrospinal fluid). A cisternogram is a test in which the flow of cerebrospinal
fluid can be monitored. This is done by injecting a substance into the cerebrospinal fluid by inserting a
needle in the spinal canal. The substance flows throughout the cerebrospinal fluid and emits a signal. A
scanner detects the signal and provides information about the flow of cerebrospinal fluid. It should be
noted that although cisternograms were used in the past, they are usually not used now days.
Although the results of CT scans, MRIs, and cisternograms may be consistent with normal pressure
hydrocephalus, they may also be consistent with other conditions. Thus, these tests are not sufficient
for a diagnosis of normal pressure hydrocephalus. CT and MRI scans will usually show widening of the
ventricles. However, it is important to note that many normal elderly people have widened ventricles.
Another common findings on a CT scan for people with normal pressure hydrocephalus include a
normally sized subarachnoid space (see previous section). A CT scan may also show that
cerebrospinal fluid is flowing through the ependyma, which is a type of membrane that lines the
ventricles of the brain.
On an MRI scan, one may see that the corpus callosum is thinned and pushed upwards. The corpus
callosum is a large band of nerve fibers in the brain that helps the two sides of the brain communicate
with each other. Also on an MRI, there may be flow voids present in the cerebral aqueduct and third
ventricle. A flow void is a loss of signal in a structure that normally has fluid flowing through it, indicating
that there is lower than normal levels of fluid in the structure. Remember from above that the cerebral
aqueduct is a narrow opening in the brain that connects the third ventricle with the fourth ventricle,
allowing cerebrospinal fluid to flow between these two areas.
The frontal horns of the lateral ventricles may appear rounded in patients with normal pressure
hydrocephalus. The frontal horns are the front parts on each side of the lateral ventricles. The results of
a spinal tap reveal usually reveals that the cerebrospinal fluid pressure is normal. As a result of the
difficulty diagnosing normal pressure hydrocephalus, this condition often goes untreated.
In addition to results of brain scans, the main thing that health care providers focus on are the three
main signs discussed above. These signs are difficulty walking, difficulty thinking, and difficulty holding
in urine. Even these signs, however, are not specific to normal pressure hydrocephalus and can be due
to other conditions.
HOW IS NORMAL PRESSURE HYDROCEPHALUS TREATED?
If a cause for normal hydrocephalus can be identified, the condition can often be treated and the effects
can often be reversed. The most common type of treatment is called a shunt. A shunt is a flexible tube
that is inserted into the ventricle, which drains the extra cerebrospinal fluid.
The most commonly used shunt is called a ventriculperitoneal (VP) shunt because it drains
cerebrospinal fluid from the ventricles to the peritoneum. The peritoneum is a layer of tissue that lines
the belly and covers most of the organs in the belly. Another type of shunt is a ventriculoatrial shunt, so
named because it drains cerebrospinal fluid from the ventricles to the atrium of the heart. Each chamber
on the top of the heart is called an atrium
A shunt may be placed even if the physician is not certain that the cause of the patient's problems is
normal pressure hydrocephalus. The decision on whether to place a shunt will be based on the results
of a clinical evaluation by the doctor and the results of a CT scan. If the condition improves after
placement of a shunt, health providers are generally confident that the cause of the patient's problems
was normal pressure hydrocephalus. It is worth noting that shunting can help decrease the size of the
ventricles in 3 to 4 days even if the hydrocephalus has been present for a year, and sometimes more.
Temporary relief of symptoms may be achieved with a spinal tap or treatment with Acetazolamide
(Diamox). Acetazolamide is a diuretic medication that can decrease the production of CSF. A diuretic is
a medication that helps to release fluids from the body in the form of urine. There is no definitive
evidence yet, however, that medication can effectively treat normal pressure hydrocephalus.
WHAT IS THE PROGNOSIS FOR PEOPLE WITH NORMAL PRESSURE HYDROCEPHALUS?
Prognosis will also depend on whether there are other co-occurring diseases (see above) of the brain
present in addition to normal pressure hydrocephalus. In generally, however, prognosis is generally
determined by the effectiveness of the shunt. It has been estimated in one large study that only about
21% of patients improve after shunt surgery (see last section). In this same study, approximately 28%
of patients experienced some type of complication. Thus, shunt surgery is not a guarantee that
significant improvement will occur and is not without risks. On a more positive note, some studies have
found that as many as 80 percent of individuals can improve after shunt surgery. The findings differ
based on the number of patients, type of patients, causes of hydrocephalus, and operative
techniques/procedures used in the study.
Because of the above factors, doctors need some way to determine whether shunt surgery will be
effective. This is why a presurgical evaluation is performed in which the patient is given a quick test of
cognitive (thinking) abilities and a timed walking test. Afterwards, a needle is inserted into the spinal
canal and a significant amount of cerebrospinal fluid is removed. The patient is then readministered the
thinking test and asked to do the timed walking test again. A clear improvement in either of these two
tests indicated that the patient will respond well to shunt surgery. Decreased urges to urinate or
increased bladder control may also indicate that shunting will be an effective treatment. The previously
mentioned changes may not occur immediately, but may take 1 to 2 days. The presurgical procedure
may be repeated over the next day or two if the patient is a good candidate for a shunt. When
presurgical evaluations are performed to select patients for surgery, more than half of the patients can
show a significant improvement after the shunting procedure is performed.
If the shunting procedure is performed, it may take about 3 days for symptoms to improve but can take
as long as a few weeks. Mental abilities and control of urine improve quicker than walking abilities after
a shunting procedure is performed. However, dementia of longer than two years is less likely to
reverse. If the shunting procedure was not effective, it may need to be revised with an additional
surgery.
If a cause of normal pressure hydrocephalus cannot be identified and/or the shunting procedure does
not work, the condition often gets worse and can lead to a progressive dementia and death. Death can
occur because the extra cerebrospinal fluid can press on the brainstem, an area of the brain that
controls many crucial life functions, such as breathing. One study showed that death and persistent
disability occurs in about 7% of patients after shunting.
WHEN WAS NORMAL PRESSURE HYDROCEPHALUS FIRST DESCRIBED?
Normal pressure hydrocephalus was first described in 1965 by Dr. Solomon Hakim while he was
training in neurosurgery (surgery of the brain and/or spine) at Massachusetts General Hospital.
HOW IS NORMAL PRESSURE HYDROCEPHALUS ABBREVIATED?
Normal pressure hydrocephalus is often abbreviated in medical charts as NPH.
WHAT ELSE IS NORMAL PRESSURE HYDROCEPHALUS KNOWN AS?
Normal pressure hydrocephalus is also known as occult hydrocephalus and Hakim's disease.
WHAT IS THE ORIGIN OF THE TERM, NORMAL PRESSURE HYDROCEPHALUS?
Normal pressure hydrocephalus comes from the Latin word "norma" meaning "rule," the Latin word
"premere" meaning "to press," the Greek word "hydor" meaning "water," and the Greek word "kephale"
meaning "head." Put the words together and you have "rule to press water head," which doesn't make
much sense in the literal translation unless you read about what it is.